Blood in the stool typically means an individual is bleeding somewhere in their digestive system. The occurrence can be frightening and anxiety provoking. Signs of bleeding may include seeing it on toilet paper upon wiping after a bowel movement, on the outside of a bowel movement, in the toilet water after a bowel movement, or on an occult blood test ordered by a healthcare provider. The color can range from bright red to dark maroon to dark black. The etiology of blood in the stool can range from benign (noncancerous) to malignant (cancerous).
12 causes of blood in the stool are…
1. Hemorrhoids
Hemorrhoids represent swollen and inflamed veins in the anus and lower rectum. They can be caused by a variety of factors including straining during bowel movements, obesity, pregnancy, prolonged sitting, chronic constipation, and a low-fiber diet. Hemorrhoids can be internal or external. Internal hemorrhoids are located above the rectum and are typically painless. External hemorrhoids occur under the skin around the anus and can be exquisitely painful. Damage to the delicate surface of a hemorrhoid may cause it to bleed.
Signs and symptoms of hemorrhoids may include blood in the stool, itching or irritation in the anal region, and a painful swelling or lump around the anus. The Mayo Clinic estimates just about 50-percent of adults have experienced hemorrhoid symptoms by the age of 50. Mild hemorrhoid symptoms are typically treated with over-the-counter agents. Severe hemorrhoid symptoms may require medical procedures such as removal of the hemorrhoid, rubber band ligation, sclerotherapy, laser therapy, or stapling.
2. Anal Fissures
Anal fissures are small tears in the skin of the anus. The usual cause of anal fissures is trauma from the passage of very hard or large stools, but they may also be caused by constipation, straining during bowel movements, chronic diarrhea, and childbirth. Anal fissures are very common. They can be acute (healing in < 8-weeks) or chronic (not healed after 8 to 12-weeks). Chronic anal fissures may need medical or surgical treatment.
Signs and symptoms of anal fissures may include itching, pain with bowel movements, and blood in the stool. Some individuals suffer from pain secondary to spasm of the anal sphincter, or ring of muscle at the end of the anus. Diagnosis of anal fissures is made by visual inspection of the anus and canal. Most cases of anal fissures resolve with conservative over-the-counter treatments. Chronic anal fissures may need prescription medication and/or surgery (lateral sphincterotomy) to achieve healing.
3. Crohn’s Disease
Crohn’s disease is one of two recognized forms of inflammatory bowel disease (IBD). Its course is chronic, or long lasting. The disease can affect any part of the gastrointestinal (GI) tract from the mouth to the anus, although it most commonly affects the small intestine and the beginning of the large intestine, or colon. The exact cause of Crohn’s disease is unknown, but most scientists agree it is an autoimmune disease (immune system cells mistakenly attack healthy body cells).
Signs and symptoms of Crohn’s disease may include diarrhea, abdominal pain and cramping, blood in the stool, fatigue, anemia, nausea, and weight loss. Diagnosis of the disease is most commonly sought with visual examination of the colon, or colonoscopy. There is no cure for Crohn’s disease, but medication can be prescribed to reduce symptoms and improve an individual’s quality of life. Unfortunately, the disease can sometimes progress to where surgery is needed for treatment.
4. Ulcerative Colitis
Ulcerative colitis is one of two recognized forms of inflammatory bowel disease (IBD). It is a chronic (long lasting) disease of the colon, or large intestine, characterized by inflammation and tiny ulcers (open sores). Ulcerative colitis only affects the mucosa, or lining, of the colon. Most scientists agree the disease is the result of an abnormal response by an individual’s immune system, or autoimmunity.
Signs and symptoms of ulcerative colitis may include persistent diarrhea, abdominal pain, blood in the stool, fatigue, loss of appetite, and weight loss. Ulcerative colitis can easily be diagnosed via colonoscopy, or visual examination of the colon. There is no known cure for ulcerative colitis. Therapy is geared toward prescription medication that suppresses inflammation and allows healing of the colon. Medical therapy is not successful in up to 25-percent of individuals with ulcerative colitis. At that point, surgical intervention may be needed to remove parts of the colon (colectomy).
5. Ulcerative Proctitis
There are different types of ulcerative colitis, one of them being ulcerative proctitis. This form of the disease consists of fine ulcerations in the inner mucosal lining of the large intestine. Inflammation first appears at the rectum and spreads a bit into the colon, but does not penetrate the bowel muscle wall.
In almost every case of ulcerative proctitis, blood appears in the stool. This is because all symptoms relate to the rectom. These symptoms include diarrhea, constipation, discomfort after having a bowel movement, and the feeling of incomplete emptying of the bowels. This disease can be managed with a combination of lifestyle changes, symptomatic medication therapy, anti-inflammatory medication therapy, and possibly surgery.
 Aksabir / Shutterstock
Aksabir / Shutterstock6. Angiodysplasia
Angiodysplasia is the most common vascular abnormality of the digestive system and represent small vascular abnormalities called arteriovenous malformations (AVMs) on the walls of the colon. Angiodysplasia is more common in older adults, especially individuals older than 60-years. It almost exclusively occurs on the right side of the colon. The exact cause of angiodysplasia is unknown. It is the most common cause of recurrent lower intestinal bleeding in individuals with kidney failure.
Signs and symptoms of angiodysplasia may include blood in the stool with no associated pain, fatigue, shortness of breath, and anemia. The blood vessels in AVMs are fragile and more apt to bleed. Angiodysplasia may be diagnosed via colonoscopy, or visual examination of the colon. Treatment entails cautery or argon plasma coagulation, which are two procedures used to control bleeding. Occasionally, surgery is needed to remove the entire right side of the colon (right hemicolectomy).
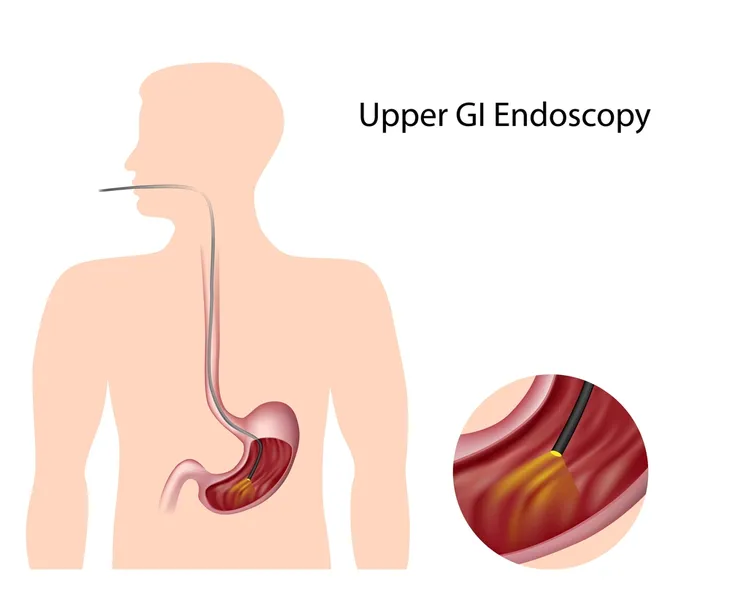
7. Peptic Ulcers
Peptic ulcers refer to open sores caused by exposure to stomach acids. The most common types of peptic ulcers occur in the stomach (gastric ulcer) and duodenum (duodenal ulcer). The duodenum is the first portion of the small intestine. Individuals may have both types of peptic ulcers at the same time. Peptic ulcers are caused by infections with the bacteria Helicobacter pylori or the use of non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, or naproxen.
Signs and symptoms of peptic ulcers may include boring-type upper abdominal pain, nausea, vomiting, blood in the stool, bloating, fatigue, shortness of breath, and lightheadedness. Diagnosis of peptic ulcers is readily made by visualization on upper endoscopy (a scope to view the esophagus, stomach, and duodenum) or upper GI series (X-rays of these areas with contrast). Peptic ulcers associated with H. pylori are typically treated with acid suppression therapy and triple antibiotics.
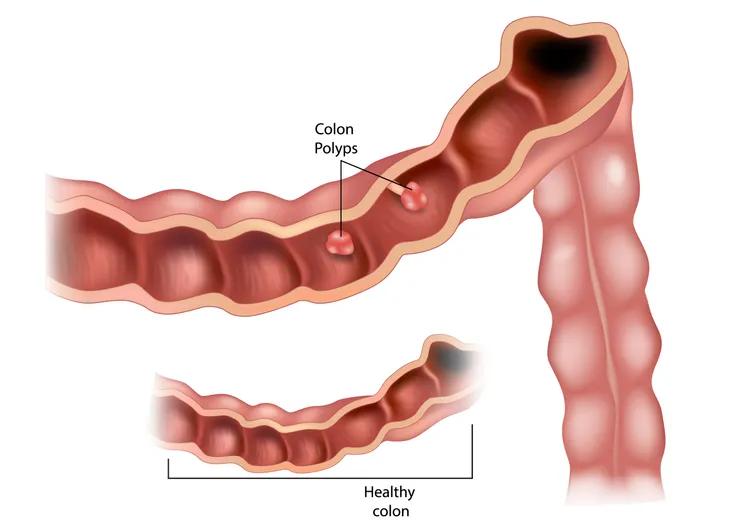
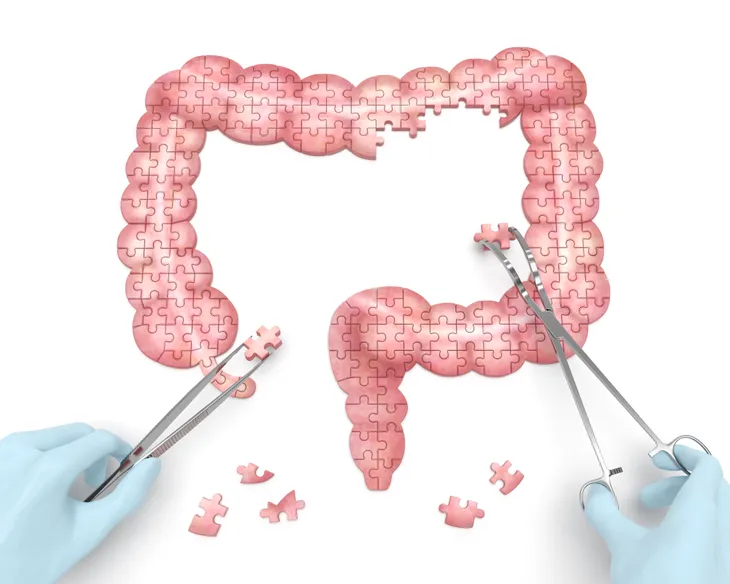
8. Colon Polyps
Colon polyps are growths in the inner lining, or mucosa, of the colon, or large intestine. It has been well established that colon cancers develop from colon polyps. The three primary types of colon polyps are hyperplastic, inflammatory, and adenomatous. The vast majority of colon polyps are benign (not cancerous), but adenomatous colon polyps have the greatest potential to turn into colon cancer.
Signs and symptoms of colon polyps may include blood in the stool, constipation, and diarrhea. Most colon polyps do not produce any signs or symptoms, which makes colon cancer screening with colonoscopy at age 50 very important. Colonoscopy allows for removal of colon polyps for microscopic analysis. In some instances, removal of the colon polyp is therapeutic and prevents the development of colon cancer in the future. Colon polyps rarely recur once completely removed.
9. Diverticular Disease
Diverticular disease affects the lining of the colon. It encompasses diverticulosis, diverticulitis, and diverticular bleeding. Diverticulosis refers to the development of small pouches, called diverticula, in weakened areas of the colon. In the United States, it is estimated that half of all individuals over age 60 have diverticulosis. No one is exactly sure what causes the disease, but some scientists think it may be linked to a low-fiber diet. Most individuals with diverticulosis do not have symptoms.
Occasionally, the pouches become inflamed and infected (a condition called diverticulitis). Signs and symptoms of diverticulitis may include severe abdominal pain, fever, and nausea. Occasionally, a blood vessel may burst near diverticula and cause blood in the stool. Diverticular disease is usually diagnosed during colon cancer screening via colonoscopy, barium enema, or flexible sigmoidoscopy. Diverticulitis is treated with dietary restrictions and antibiotics. Severe cases of diverticulitis or diverticular bleeding may require surgery to remove parts of the colon.
10. Colon Cancer
Colon cancer is a malignant tumor arising from the mucosa, or inner lining, of the colon. It is the third most common cancer diagnosed in the United States. Risk factors for colon cancer include a family history of colon cancer, colon polyps (specifically adenomatous colon polyps), and ulcerative colitis. Most colon cancers develop from colon polyps, which makes colon cancer screening paramount at age 50. The removal of colon polyps can prevent colon cancer.
Signs and symptoms of colon cancer may include diarrhea, constipation, narrowing of the stool, blood in the stool, abdominal pain, weakness, and weight loss. Screening for colon cancer may be accomplished with a fecal occult blood test, sigmoidoscopy, barium enema, or colonoscopy. Colonoscopy is ideal because abnormal lesions can be biopsied and categorized as precancerous, malignant (cancerous), or benign (noncancerous). Surgery is the most common treatment for colon cancer.
11. Ischemic Colitis
Ischemic colitis refers to a reduction in or total obstruction of the blood flow to a particular section of the colon. It is typically caused by a narrowed or blocked artery and culminates in reduced oxygen to the cells of the colon. A reduction in or total obstruction of the blood flow to the colon can quickly lead to the death, or necrosis, of the colon. Risk factors for ischemic colitis include advancing age, clotting abnormalities, and surgery on the aorta.
Signs and symptoms of ischemic colitis may include abdominal pain and cramping, blood in the stool, diarrhea, and nausea. Diagnosis of ischemic colitis can be made with X-rays of the blood vessels (angiography) of the colon and/or colonoscopy. There are no particular recommendations for the prevention of ischemic colitis. Treatment depends on the severity of the disease and can entail antibiotics, intravenous fluids, treating any underlying medical conditions, and surgery.
12. Blood in Children’s Stool
It’s also possible for blood to appear in your child’s stool. The most common reason for 90 percent of cases according to Seattle Children’s Hospital is an anal fissure. This is typically caused when they pass a large or hard stool. Other possible reasons include Strep skin infection, bacterial diarrhea, and cow’s milk colitis in babies.
13. Symptoms of Blood in Stool
If you find blood in the stool, it’s possible your body is experiencing other symptoms as well. Certain symptoms may give doctors an idea of what the underlying cause is before you go through testing.
Symptoms often present in conjunction with blood in the stool are:
- Abdominal pain
- Fatigue
- Weakness
- Shortness of breath
- Pale skin
- Rectal pain
14. Appearance of Blood in Stool
Blood in the stool can appear in various different ways. You may notice blood on toilet paper when you wipe, see blood in the toilet bowl after using it in the bathroom, or noticing a difference in the actual color of your stool. If your stool is discolored, there are a few ways it might look. Stool could have bright red streaks on it or mixed within it. Alternatively, the stool could look dark and tarry.
15. Blood in Stool May Not Always Be Visible
Some people may have blood in stool but not even realize it. This is because small amounts of blood are not visible to the naked eye and can only be seen under a microscope. In this case, the blood may be discovered during a lab test and not be the initial reason why you’re seeing the doctor.
 Konstantin Kolosov / Shutterstock
Konstantin Kolosov / Shutterstock16. Risk Factors
Anyone can develop blood in the stool, but you may have increased risk of this happening depending on your health history.
Factors that increase your risk for blood in the stool include:
- A history of stomach bleeding or hemorrhoids
- Had previous peptic ulcers
- Undiagnosed or diagnosed inflammatory bowel disease
- Genetic risk of colorectal or upper GI cancers
17. Diagnosing Blood in Stool
Doctors will take into account a patient’s health history, various symptoms, and severity of condition when diagnosing the reason behind blood in the stool. From there, further testing may be ordered.
One possible test is a nasogastric lavage. This involves removing the contents of the stomach through a tube to find out whether there is blood in the stomach. Other tests that could be ordered are barium x-rays, angiography, or more invasive options such as an endoscopy, colonoscopy or laparotomy.
18. Treatments for Blood in Stool
There are several techniques a doctor may recommend to treat bloody stool. It will ultimately be determined by the current state of the patient and the results found from testing.
- Stop the bleeding — doctors may be able to control bleeding with procedures such as an endoscopy or angiography.
- Medication — certain drugs may be prescribed to treat ulcerative colitis or another disease treatable by medication.
- Surgery — some patients may require surgery to remove polyps or parts of the colon damaged by disease.
- Lifestyle changes — consuming a high-fiber diet may help to relieve constipation causes by hemorrhoids and anal fissures.
- Sitz bath — sitting in warm water may help to relieve fissures and hemorrhoids.
Make sure to only pursue medical treatments that are recommended by your doctor after a proper diagnosis.
19. Possible Complications
If bloody stool is left untreated for a long period of time, Healthgrades notes of potential complications that can occur. This includes anemia, severe blood loss, or shock. The underlying cause of bloody stool could also progress and become life threatening. For example, a peptic ulcer could start to bleed. You could develop a bowel obstruction or severe abdominal trauma. To prevent further complications, you should see a medical professional as soon as possible.
20. When to See a Doctor
Blood in the stool can be a serious medical issue. It could be a symptom of conditions like ischemic colitis, angiodysplasia, or even cancer. That’s why it’s important to see a doctor as soon as you notice the appearance of blood in the stool to begin treatments.
The good news is blood appearing in the stool isn’t always a serious problem. It could be the result of an anal fissure or hemorrhoids. With proper treatment prescribed by the doctor, your stool can eventually go back to normal.