Osteoarthritis is a degenerative joint disease that affects more than 20 million people across America.
If you’ve been diagnosed with osteoarthritis, you may confuse it with other common forms of arthritis, such as rheumatoid arthritis, but the two conditions are quite different in origin. The painful inflammation associated with osteoarthritis can severely impact your mood, range of motion, energy levels, and quality of life. However, the disease is manageable once you come to understand the facts from the misconceptions. To help raise your awareness of osteoarthritis, here are fifteen common FAQs…
1. What is Osteoarthritis?
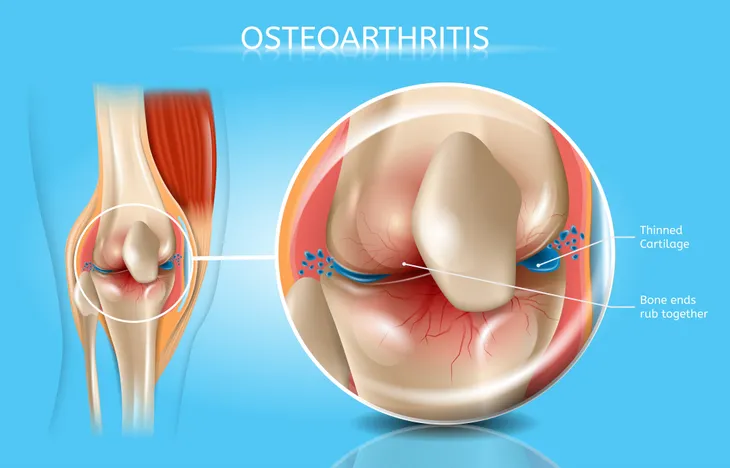
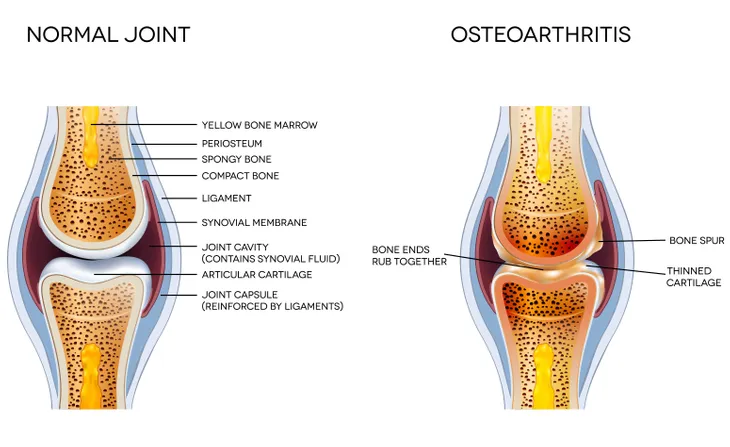
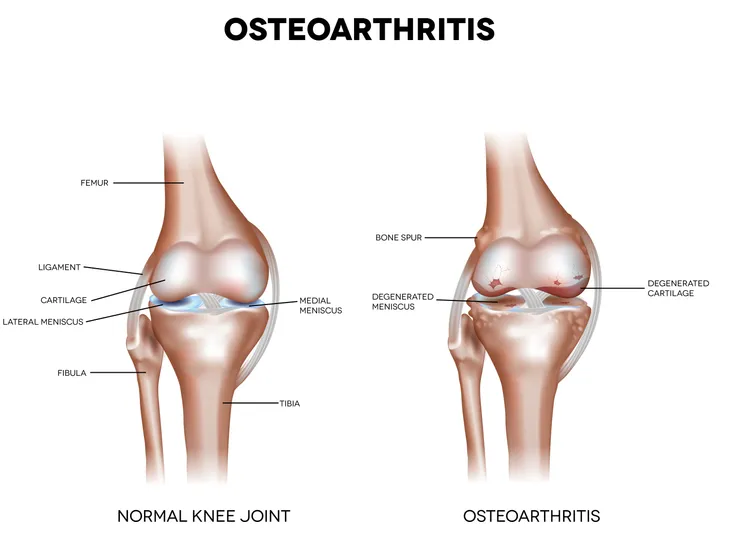
Osteoarthritis is the most common form of “wear-and-tear” arthritis, which refers t the way the disease gradually breaks down cartilage, or the protective covers over the ends of our bones that allows for smooth and pain free joint movement.
With osteoarthritis, cartilage wears away, bones spurs can form, and joints rub against each other, causing pain, inflammation, stiffness, excruciating movement.
2. How Many People Have Osteoarthritis in the U.S.?
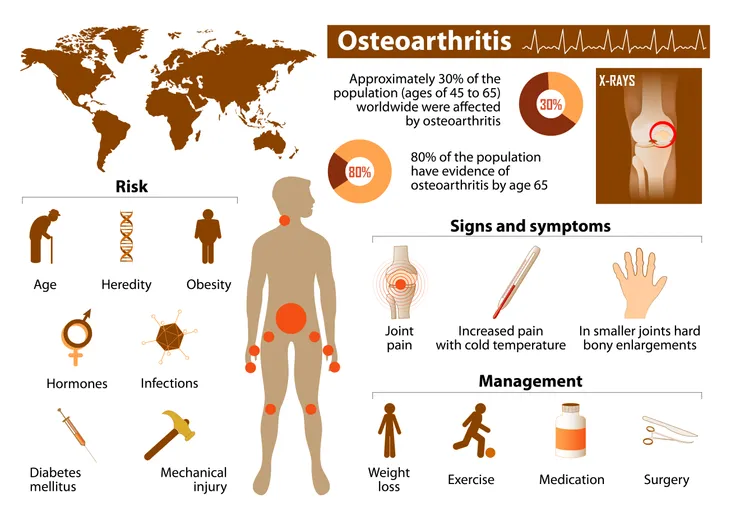
Osteoarthritis is the most common arthritis in North America. This degenerative disease impacts nearly 27 million people across the U.S. Osteoarthritis is more common in middle-aged to senior females.
However, middle-age to senior males are also at risk for osteoarthritis due to weight gain, age and following an injury.
3. Difference Between Rheumatoid Arthritis vs. Osteoarthritis?
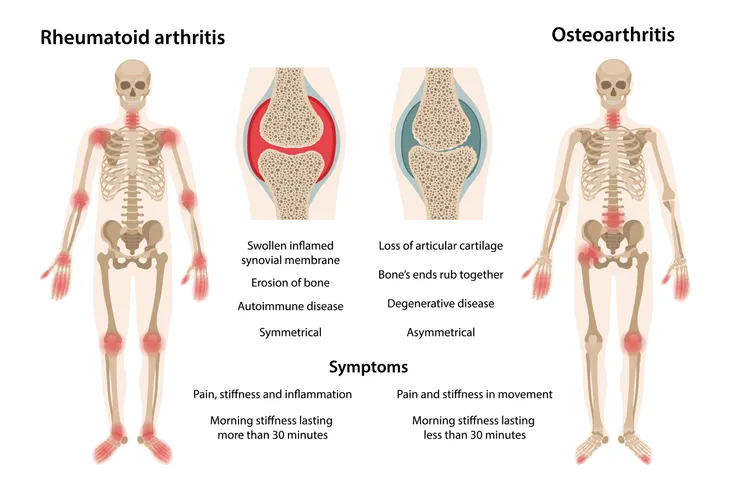
There is some confusion between rheumatoid arthritis vs. osteoarthritis due to the simple fact that both attack the joints. However, the cause and treatment between the conditions differ in these ways:
- Rheumatoid arthritis is an autoimmune disease, which means the immune system attacks the joints, causing inflammation, pain, and stiffness. Rheumatoid arthritis typically impacts the hands, wrists, and feet. A doctor will typically prescribe medications to suppress the immune response and ease joint attacks.
- Osteoarthritis is a degenerative joint disease, which wears away at the cartilage, or cushioning, surrounding a healthy joint, causing bone spurs to develop and rub against one another, making movement painful, stiff, and causing inflammation. Osteoarthritis typically appears in weight bearing joints such as the knees, hips, fingers, hands, neck, lower back, and ankles.
4. What Causes Osteoarthritis?
While no single cause is known, osteoarthritis can result in those who are obese.
Osteoarthritis is also common to those have incurred a joint injury, those prone to jobs with repetitive stress, due to heredity, as well as age.
5. Risk Factors for Osteoarthritis
The following factors are common ones in osteoarthritis patients:
- Heredity—if joint birth defects or joint disease runs in your family
- Obesity—carrying around excess weight adds stress to the joints and can prompt injury, cartilage damage, and eventually osteoarthritis
- Injury—a traumatic injury or repetitive stress injury that causes ligament or joint damage may eventually lead to osteoarthritis
- Gender—women are more prone to osteoarthritis compared to men
- Muscle weakness around a joint can put you at risk of injury and eventually, osteoarthritis
- Spinal issues—such as Scoliosis or curvatures of the spine
- Advanced age—osteoarthritis most commonly strikes those in middle-age to those in their senior years
6. Symptoms of Osteoarthritis
As a degenerative disease, osteoarthritis develops gradually over time—meaning you may only experience moderate symptoms at first, but eventually, the disease will cause severe inflammation, pain, and stiffness that affect your quality of life in these ways:
- “Morning stiffness”, which usually occurs upon waking or after lengthy periods of inactivity
- Pain caused by rubbing of joints
- Inflammation due the bone spurs and painful rubbing of joints
- Difficult, painful movement (i.e., walking, bending over, getting up from seating, climbing stairs, and standing)
7. How is Osteoarthritis Diagnosed?
To make a proper osteoarthritis diagnosis, your physician examines your medical history and performs a physical exam that may include x-rays, MRIs, and blood tests.
If osteoarthritis is suspected, the patient is referred to a rheumatologist (a health professional that specializes in joint health).
8. Common Osteoarthritis Treatments?
Osteoarthritis treatments vary according to the following factors:
- Your age
- Family history
- General health
- Severity of injury
- And arthritis acuteness (or stage)
As a result, your osteoarthritis treatment program could include one or more of these treatments:
- Over-the-counter pain relievers
- Assistive devices (i.e., cane, walker, or crutches)
- Hot/cold compresses
- Exercise, diet to control weight
- Prescription medication
- Surgery (in severe cases)
9. Lifestyle Changes That Will Relieve Osteoarthritis Pain
Weight Loss—a healthy diet and low-impact exercise program can help you lose and maintain a healthy weight to lessen stress on the joints.
Rest and relaxation—will help ease joint pain as well as the depression and hopelessness that can come with a loss in quality of life. Gentle yoga breathing, massage, meditation with guided imagery may be recommended by your doctor to relax your body and mind. Check out these lifestyle tips to manage and prevent osteoarthritis!
10. Common Prescription Treatments for Osteoarthritis?
To treat osteoarthritis pain, a doctor will typically prescribe medications to ease pain and inflammation on the joints such as:
- Nonsteroidal anti-inflammatory medications (or NSAIDs). Also, oral or patch prescription NSAIDs are also common if over-the-counter versions don’t alleviate pain.
- Analgesics can aid in pain relief.
- Topical gels, ointments, creams, and sprays to reduce swelling in joints.
- COX-2 Inhibitors manage pain when NSAIDs cause severe stomach upset and risk of stomach ulcers and bleeding.
- Prescription pain medications.
- Antidepressants—to ease depression associated with chronic pain.
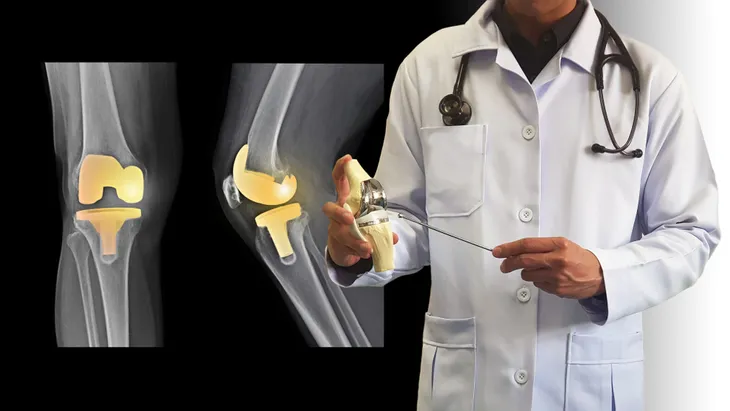
11. What Surgeries are Recommended for Osteoarthritis?
The following two surgeries are only typically recommended in severe osteoarthritis cases, firstly, arthroplasty removes a portion of bone, realigning the joint in order to replace or restore a severely damaged joint and improve mobility and quality of life.
The second surgery option is cartilage repair and regeneration, which replaces damaged cartilage for those with severe and painful cartilage defects.
12. When Should I Consider Surgery?
A physician will typically only resort to surgery if all other treatments for osteoarthritis fail and an individual is virtually in severe pain and left disabled due to loss of range in joint motion.
Again, surgery will depend on the patient’s age, activity level, family history, and the joint affected.
13. Complementary or Alternative Therapies for Osteoarthritis?
Alternative therapies such as chiropractic manipulation, acupuncture, massage, gentle yoga, or herbal remedies may provide pain relief to a painfully damaged joint.
However, please keep in mind that alternative therapies should be used in conjunction with your family physician.
14. Will Exercise Improve Flexibility, Strength, and Relieve Pain?
Yes, gentle exercise can help manage osteoarthritis pain and increase range of joint flexibility, strength, and motion.
It will also promote positive energy and mood. Just be sure to consult with your physician or physical therapist before exercising.
15. How to Prevent Osteoarthritis
Even if you are prone to osteoarthritis due to heredity, injury, gender, or age, you can proactively do your part to prevent the onset by doing the following:
- Consuming a healthy, balanced diet
- Maintaining a healthy weight
- Exercising regularly
- Getting adequate sleep