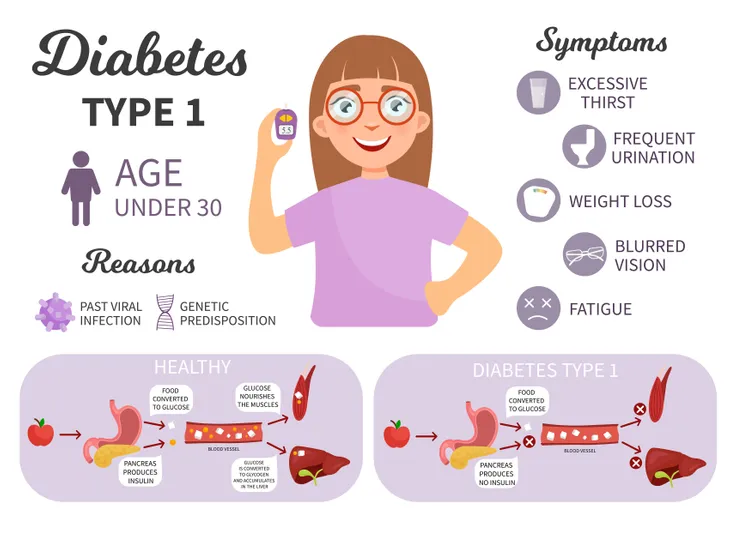
While symptoms can show very early on, type 1 diabetes shares many symptoms with other conditions and disorders, making it hard to personally diagnose. This is why it’s important to not only take notice of any changes in your body, but also get checked by your doctor at the first sign of anything that could even remotely be related to type 1 diabetes.
Common Symptoms
To understand what to look for when it comes to symptoms associated with type 1 diabetes, keep watch for any of these symptoms, as listed by the Mayo Clinic:
- Excessive urination or bed-wetting in children (the result of your kidneys trying to expel excess sugar in your blood).
- Feeling very thirsty, experiencing a dry mouth, or having itchy skin (due to the dehydration caused by your kidneys trying to expel excess sugar in your blood).
- Feeling very tired or weak, increased hunger (especially after eating), unintended weight loss, or loss of muscle bulk (due to your body not getting adequate energy from the food you eat).
- Frequent or recurring infections, slow-healing cuts or bruises, tingling or numbness in the hands or feet, or difficulty getting or maintaining erections in men (due to high blood sugar levels affecting blood flow and causing nerve damage, which in turn makes healing difficult).
- Frequent yeast infections (due to yeast infections feeding on glucose).
- Blurred vision (due to the lens of your eye changing shape).
Severe Symptoms
As explained by EndocrineWeb, more serious cases of type 1 diabetes, signs and symptoms can include:
- Loss of appetite
- Nausea or vomiting
- Low body temperature (below 97º F)
- Rapid, heavy, labored breathing (sometimes called Kussmaul respiration)
- Stomach pain
- Shaking and confusion
- Fruity, potentially pear-smelling breath (due to high ketones, a result of ketoacidosis)
- Loss of consciousness (this is rare)
- Changes to (or loss of) menstruation in women
- Reduced blood pressure (falling below 90/60)
- Hypoglycemia (low blood glucose)
- Hyperglycemia (high blood glucose)
If you experience any of these signs or symptoms, you should seek immediate medical attention.
Short-Term Complications of Type 1 Diabetes
Not seeking medical attention can lead to more severe complications. These complications can be both short- and long-term and affect the nerves, heart, blood vessels, eyes, and kidney.
Hypoglycemia
Hypoglycemia happens when the body doesn’t have enough of the hormone that regulates glucose in your blood causes your blood sugar levels to drop too low. There are also three levels of hypoglycemia, depending on how severely your blood glucose level has dropped: mild, moderate, and severe. Serious problems caused by hypoglycemia can usually be avoided if treated in the mild or moderate levels, but the repercussions of severe hypoglycemia can be far more serious, including falling into a coma and even death.
Symptoms of hypoglycemia include:
- feeling shaky and irritable
- sweating
- tingling lips
- feeling weak
- feeling confused
- hunger
- nausea (feeling sick)
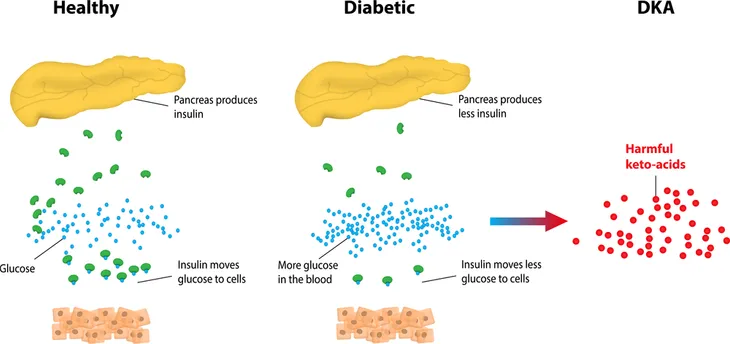
Diabetic Ketoacidosis
Diabetic ketoacidosis (DKA for short) is another serious complication that happens when your body can’t effectively use glucose as a form of energy and instead begins breaking down fat to use as energy. This results in what are called ketones being released into your blood, which, if left untreated, can make your blood acidic.
Symptoms of diabetic ketoacidosis include:
- Frequent urination
- Extreme thirstiness
- Abdominal pain
- Weight loss
- Fruity, potentially pear-like smell on breath
- Cold skin
- Confusion
- Weakness
Long-Term Complications of Type 1 Diabetes
Generally speaking, these long-term complications, which usually develop over a period of at least 10 years, belong to two categories: microvascular and macrovascular complications.
Microvascular Complications: Eye, Kidney, and Nerve Disease
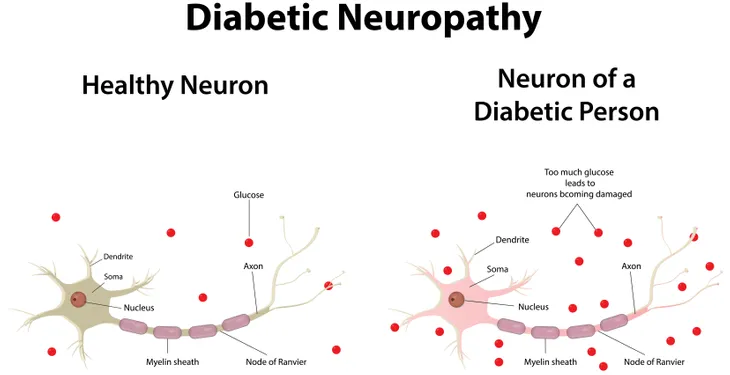
Diabetes, which is defined by poor to no blood glucose control, can result in damaged blood vessels that don’t deliver blood as they should, which leads to problems with the eyes, kidneys, and nerves.
Eyes: Type 1 diabetes can cause cataracts and/or retinopathy to develop in your eyes. Either one can result in loss of vision, says WebMD.
Kidneys: WebMD also notes that poorly controlled type 1 diabetes will likely eventually cause the kidneys to fail and lead to the need for dialysis and/or a kidney transplant.
Nerves: Nerve damage caused by diabetes, aka diabetic neuropathy, makes it more difficult for tiny blood vessels to nourish your nerves. This can lead to nerves, most commonly in your feet, not functioning properly. This can also lead to such things as erectile dysfunction in men.
Macrovascular Complications: The Heart
By causing damage to large blood vessels, type 1 diabetes can also cause plaque to build up resulting in cardiovascular problems, says WebMD, like coronary artery disease with chest pain (angina), heart attack, stroke, narrowing of the arteries (atherosclerosis), and high blood pressure.
Causes
Type 1 diabetes is the result of your body’s own immune system mistakenly destroying the beta cells in the pancreas, resulting in the inadequate production of the hormone that regulates glucose in the blood. Unlike type 2 diabetes, type 1 diabetes isn’t caused by diet and lifestyle habits (although diet and lifestyle can positively or negatively affect type 1 diabetes once you have it).
While glucose is required by your body as a main source of energy for the cells that make up muscles and other tissues, the buildup of glucose in your bloodstream instead of the absorption of glucose by your cells, as happens to type 1 diabetics, has potentially life-threatening effects.
Although it’s not entirely understood what causes type 1 diabetes, possible causes are believed to be genetics and exposure to viruses and other environmental factors, explains the American Diabetes Association. However just because a parent passes down genes associated with type 1 diabetes to their children doesn’t necessarily mean that those children will develop type 1 diabetes.
Risk factors
Risk factors for type 1 diabetes are not as clear as risk factors for prediabetes and type 2 diabetes.
However, according to Mayo Clinic and EndoctrineWeb, some known risk factors for type 1 diabetes include:
- Family history: Anyone with a parent or sibling with type 1 diabetes has a slightly increased risk of developing the condition. This risk is higher when the father has type 1 diabetes, and even higher when both parents have type 1 diabetes.
- Genetics: The presence of a certain genetic marker indicates an increased risk of developing type 1 diabetes. That genetic marker is located on chromosome 6, and it’s an HLA (human leukocyte antigen) complex.
- Age: Although type 1 diabetes can appear at any age, it appears at two noticeable peaks. The first peak occurs in children between 4 and 7-years-old, and the second is in children between 10 and 14-years-old.
- Viral infections: Certain viruses may trigger the development of type 1 diabetes by causing the immune system to turn against the body—instead of helping it fight infection and sickness. Viruses that are believed to trigger type 1 include German measles, coxsackie, and mumps.
- Race/ethnicity: Certain ethnicities have a higher rate of type 1 diabetes. In the United States, Caucasians seem to be more susceptible to type 1 than African-Americans and Hispanic-Americans. Chinese people have a lower risk of developing type 1, as do people in South America.
- Other autoimmune conditions: There are other autoimmune conditions that may share a similar HLA complex, and therefore, having one of those disorders may make you more likely to develop type 1. Other autoimmune conditions that may increase your risk for type 1 include Graves’ disease, multiple sclerosis, and pernicious anemia.