You’re doubled over in pain from something happening in your abdomen, and your mind might automatically go to the worst case scenario. However, while it may be something serious, in most cases, it’s not.
It’s important to know the difference between appendicitis – an emergency medical condition that can be fatal – and when you’re experiencing the result of excessive gas. Let’s take a look at 12 differences between the two…
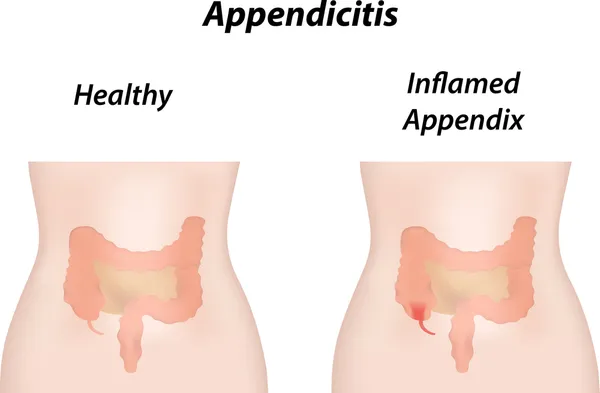
1. The Low Down on Appendicitis
Appendicitis occurs when the appendix – which typically is located in the lower right abdomen, becomes inflamed and filled with pus, “a fluid made up of dead cells that often results from an infection,” notes EveryDay Health.
If you don’t get medical attention for this painful condition, your appendix may burst, spreading the infection throughout your abdomen (a condition called peritonitis) that can result in death.
2. Triggers for Appendicitis
We normally don’t give our appendix a second thought, that is, until it starts acting up and causing us problems. So what can cause appendicitis?
According to MedicineNet.com, appendicitis often occurs when the organ becomes blocked, whether by stool, a foreign body, or even cancer. The blockage may also be the result of an infection, “since the appendix swells in response to any infection in the body,” adds the source.
3. Gas Isn’t a Breeze
Unlike appendicitis, gas is common and isn’t the result of an infection. But that doesn’t mean it isn’t potentially painful and alarming. The Mayo Clinic explains that gas forms when bacteria in the colon ferment carbohydrates that haven’t been digested in your small intestine.
Gas can catch people off guard, because, as the source explains, “Unfortunately, healthy, high-fiber foods are often the worst offenders.” Fiber (from sources such as fruits, vegetables, beans, and whole grains) is important in keeping the digestive tract in good working order, but gas is often an unwanted side effect.
4. Measure the Pain
FindATopDoc.com explains that the level of pain may help you determine if you need to pass gas or visit an emergency room. While gas pain can be very uncomfortable, “the pain caused by simple intestinal gas can never be unbearable,” adds the source.
However, on the flipside of that coin, appendicitis can be excruciating, becoming unbearable for the patient. Have you ever seen anyone complaining of gas pain curled up on the floor groaning in pain? If you witness this, it’s probably best to call for medical assistance.
5. Shared Symptoms
In some cases, the problem is that, until you relieve the gas, you don’t know exactly what you’re dealing with. The same source explains, “Appendicitis and gas can cause a person to feel similar sensations, therefore leading to one condition being mistaken for the other.”
For example, both cause abdominal pain and potentially nausea. But again, if you find yourself doubled over in pain and unable to move, then err on the side of caution and call a doctor.
6. Location is Key
Along with the level of pain, the exact location of the pain and how it spreads can be another key clue in determining if you’re dealing with gas or appendicitis.
WebMD notes that the “classic symptoms” of appendicitis include “dull pain near the navel or the upper or lower abdomen that becomes sharp as it moves to the lower right abdomen.” However, the source also points out this only occurs as a first sign in only about 50-percent of appendicitis cases. Gas, on the other hand, can present pain in various places around the abdomen and doesn’t really follow a pattern.
7. Prolonged Pain or Short Suffering?
Many gas pains will resolve fairly quickly, usually soon after you pass the gas. However, you may experience chronic appendicitis, which is considered a rare medical condition that causes pain to come and go (but can sometimes worsen).
However, when you hear about emergency cases of appendicitis, you’re hearing about acute appendicitis that can come on suddenly like bad gas pain. As Mercola.com explains, after the preliminary symptoms of appendicitis, the other symptoms will manifest within 24-hours. The appendix can rupture in 72-hours or less. Consider the last time you’ve had simple gas pain that lasted an entire day or more.
8. Gas Pains Can Be Relieved Without a Doctor
While there are DIY ways to relieve the pain and bloating associated with gas pains, such as these tips from VeryWell Health, you won’t be able to simply fix appendicitis – that’ll be up to a medical team.
If you’re displaying symptoms of appendicitis and are rushed to the hospital, doctors likely won’t give you antacid and wait it out. They’ll open you up and remove your appendix (also known as an appendectomy) to avoid possible complications.
9. Watch for Other Symptoms
While gas is usually limited to pain and sometimes nausea, you’ll likely experience other telltale signs to treat it more seriously if you’re dealing with appendicitis.
For example, WikiHow.com explains with appendix inflammation, you may also have “emergency symptoms,” such as a fever that spikes over 102-degrees Fahrenheit, back pain, decreased appetite, painful urination, or pain in the rectum.
10. Do The “Push Test”
If you have gas pain, pushing down on your abdomen doesn’t usually cause you to recoil in pain (in fact, massaging your tummy is one way to release the gas causing your problems, although there can be some tenderness during this process).
Babble.com says if you’re worried about whether it’s gas or appendicitis, especially when you’re dealing with children who can’t communicate all the symptoms, you’ll notice tender abdominal muscles, especially in that lower right area of the abdomen. There could be pain just from touching that area. However, other sources warn not to push down right at the appendix as it may increase the risk of rupture, instead push and release the opposite side and wait for a reaction. If the pain increases upon release, this may be “rebound tenderness,” which is a sign of appendicitis.
11. What Else Could it Be?
It’s possible that your abdominal pain isn’t being caused by gas or appendicitis. In fact, Medical News Today lists 15 possible reasons you might have a tender midsection.
Some of the other possible causes of your discomfort may include the stomach flu, irritable bowel syndrome (IBS), gastritis (inflammation of the stomach lining), food intolerances (e.g., lactose intolerance, inflammatory bowel disease (IBD, which includes Crohn’s, ulcerative colitis, constipation, or even a stomach ulcer).
12. Don’t Delay the Doctor
There’s one thing all the experts seem to agree on when it comes to dealing with prolonged abdominal pain that you may suspect is appendicitis – call a doctor. “Prompt surgery is often essential,” says WebMD.
The source also notes you shouldn’t eat, drink, use antacids, laxatives or heating pads to try to relieve the pain, as these can increase the risk of the appendix rupturing. Call a doctor if your appendix has already been removed but you’re experiencing abdominal pain. It could be one of the other causes we mentioned, or even pelvic inflammatory disease (PID) or a tubal pregnancy, adds the source.