Frozen shoulder, as it’s called, actually has nothing to do with the temperature. It causes pain for many people, which can be prolonged. In fact, one patient in Best Health likens it to “a lightning bolt zapping me for 20-seconds.”
The pain can shoot from the shoulder and down the arm, making it especially alarming. As the name of the condition suggests, it can also limit your range of movement. Let’s take a closer look at 12 facts about frozen shoulder…
1. What Exactly is Frozen Shoulder?
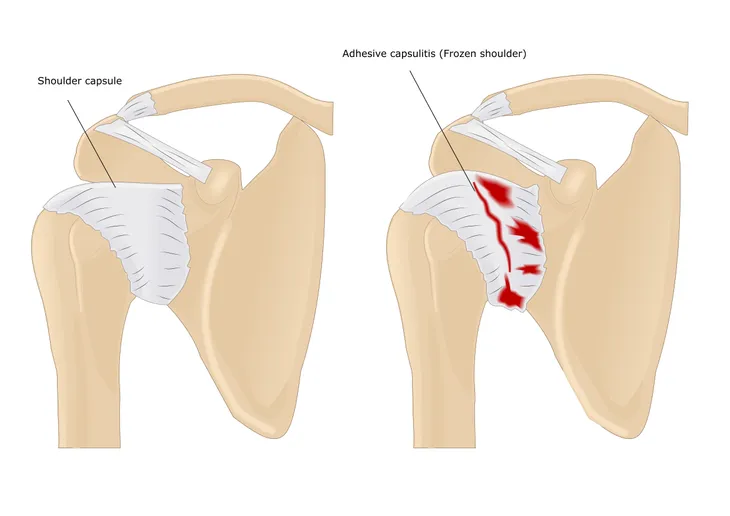
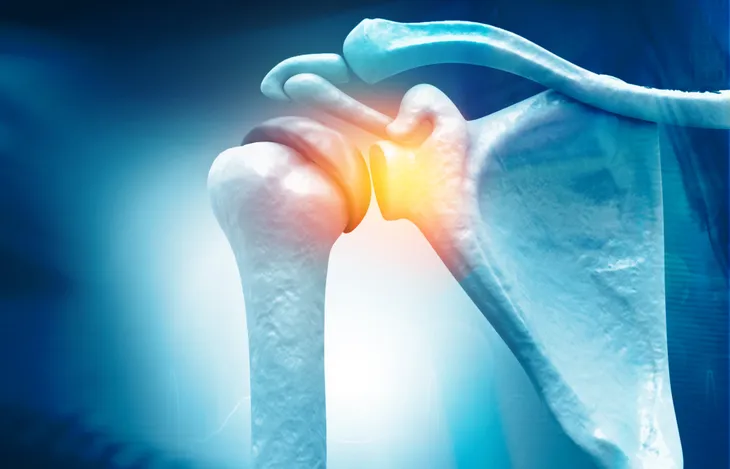
Also referred to as adhesive capsulitis in the medical world, this is caused by connective tissues around the shoulder joint becoming inflamed, leading to pain and stiffness, notes Best Health.
The condition also results in scar tissue forming inside the shoulder capsule. The condition affects about 3- to 5-percent of the population, adds the source.
2. It’s a Bit of a Cold Case
The causes of frozen shoulder are somewhat of a medical mystery. “Doctors aren’t sure why this happens to some people,” explains the Mayo Clinic, which adds that it seems to occur more often in patients with diabetes.
If you’re experiencing pain in the shoulder area and stiffness that isn’t obviously related to recent injury, you may have to visit the doctor for a diagnosis.
3. There are Three Main Stages
The Mayo Clinic also breaks the condition down into three stages, each with their own unique symptoms. The first stage is actually called the “freezing” stage, as range of motion starts to be negatively impacted.
The second stage is the “frozen” stage, which makes the joint even stiffer (but pain may actually lessen a bit by then). Finally, the “thawing” stage is when the range of motion begins to improve.
4. Causes for Concern
As noted before, the medical world is a bit stumped as to the exact causes, although there are risk factors for frozen shoulder. Medical News Today says it’s believed that frozen shoulder occurs from scar tissue forming in the shoulder, making the shoulder capsule “thicken and tighten.”
Periods of not using the shoulder can also be a cause. “Most people with frozen shoulder have experienced immobility as a result of a recent injury or fracture,” says the source.
5. Shouldering the Risks
As we mentioned earlier, it’s a bit of an unknown as to why some people develop frozen shoulder, but it’s not without its risk factors. For example, WebMD explains it’s more common in women, and more common among the 40- to 60-years age group. You may experience frozen shoulder if you’re recovering from a stroke or any surgery that limits movement of your arm (such as a mastectomy).
As noted before, diabetes is another risk factor for frozen shoulder. The source says up to 20-percent of frozen shoulder patients also have diabetes. Other linked conditions include heart disease, thyroid problems, and Parkinson’s disease.
6. Trauma Can Be a Culprit
SOSMed.com confirms all the possible causes of frozen shoulder, including diabetes and hyperthyroidism (overactive thyroid gland). But it also lists “post-traumatic” factors as possible causes.
“Shoulder or arm injury may result in a frozen shoulder from prolonged immobilization,” explains the source. It also notes that immobilization could also be the result of a “mechanical block” if bone fractures heal in the wrong position.
7. How to Shoulder the Condition
Some people may take some time getting to the doctor if they are experiencing shoulder pain, as it could be from a variety of factors. However, you shouldn’t try to function normally through the pain.
“If you think you have a frozen shoulder or are developing one, see your clinician or a shoulder expert for a physical exam,” explains an article from Harvard Medical School. In the meantime, try to limit any activities that require reaching or lifting.
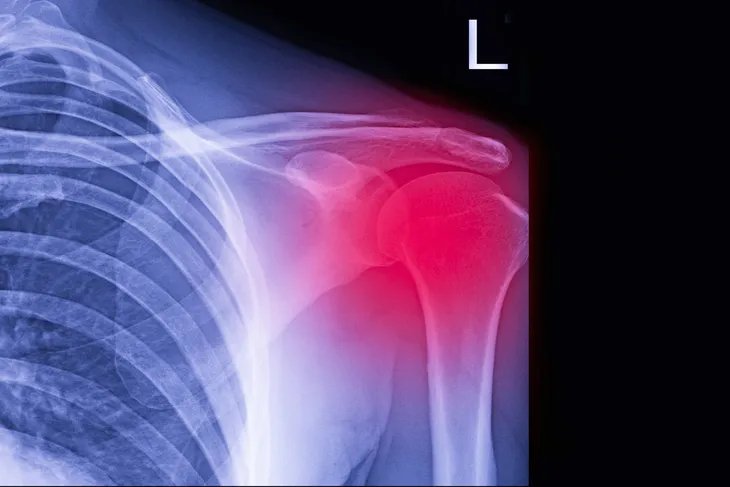
8. Diagnosis is a Joint Effort
While a doctor is an important ally to order any scans that can help rule out other causes, you can actually do some diagnostic tests of your own at home to determine if you have frozen shoulder.
FrozenShoulderClinic.com notes that patients with frozen shoulder will not be able to raise their arm more than 90-degrees without elevating the entire shoulder. Frozen shoulder is often confused with shoulder impingement syndrome, which allows for 120-degrees of arm movement, explains the source, which explains self-diagnostic tests in more detail.
9. Timeline for Thaw
The Mayo Clinic says frozen shoulder can run its course over a long period of time, with symptoms coming on gradually, then getting worse, then resolving over 1- to 3-years.
Treatment can possibly help move the healing process along, which we’ll also describe in this article. The good news is that frozen shoulder is unlikely to strike twice in the same shoulder, but it can begin again in the opposite shoulder.
10. Focus on Pain Relief
Along with the lack of mobility, pain is the biggest problem associated with frozen shoulder. To help alleviate the pain, you can turn to over-the-counter medications such as ibuprofen, explains the NHS in the UK.
In some cases where non-prescription pills aren’t doing the trick, you can turn to prescription opioids or even steroid injections to help manage swelling in the joint, notes the NHS. However, you should work closely with your doctor if you’re using prescription opioids as a solution.
11. There’s No Solid Cure
While the problem can often resolve itself over a period of time, the focus seems to be on managing the symptoms and improving range of motion through specific activities.
That means there’s no “cure” per se, but the combination of treatments (which we’ll get to next) can dramatically improve the problem and make it marginal enough to ignore.
12. Treatments Can Vary
Most sources talk about physical therapy as a solution, although the “results are mixed” on this one, says WebMD. Shoulder manipulation was widely used to free up tissue, but it has been largely abandoned due to risk of injury.
Now, arthroscopic surgery has replaced manipulation (under general anesthesia), although the need for this measure is “very rare.” This is when very small tools are inserted through tiny incisions to perform scar reducing surgery. Surgery is generally only resorted to if all other treatment options have failed.